Making Your Dreams Come True with Type 1 Diabetes
By Romain Ballet
May has always been a special month for me. 15 years ago, on May 17th 2003, I was diagnosed with type 1 diabetes. I was 16 years old. Needless to say, Type 1 is a big part of who I have become. I have built my life around type 1 and it has taught me to enjoy life to the fullest. I was always a dreamer, but before Type 1, I used to just contemplate my dreams. Now. I have started making them come true, one after the other.
The first big dream I ever realized after my diagnosis was to become a doctor in immunology. I wanted to contribute to this body of knowledge to develop medications for autoimmune diseases. I always loved the feeling of living my disease both as a patient who has to understand his blood glucose (BG), and as a scientist who has to understand its mechanisms.

The second big dream I realized was a physical achievement. Before Type 1, I was already a very active person. I played soccer as part of the Guadeloupean national team. But after my diagnosis, I decided to explore more introspective sports. During my doctorate in Geneva, I was part of a triathlon relay team. We were the Geneva Predators! My swimmer and my cyclist were so talented that I always started my runs among the first three places and my only task was to stay on the podium! I particularly enjoyed this race format because I had to get out of my comfort zone for the sake of the team.
But the real challenge came in the spring of 2014. One of my labmates told me about his wife’s recent half Ironman (1.2 miles swim, 56 miles bike ride, 13.1 miles run). I immediately started imagining myself swimming without assistance for 1.2 miles – an eternity in my mind! My first thought was: “this is impossible with type 1”. But the seed was sown and the idea of racing a half Ironman grew in me… I ended up choosing the 70.3 Ironman Pays d’Aix, in the south of France, scheduled in May 2015 (it’s always about May). At the time, I did not have my continuous glucose monitoring (CGM) and therefore had to race blind. My biggest fear was the swim, but I finished the race in 5:42:05 and proudly became a half-Ironman finisher
After that summer of 2015, I moved to Stanford University to pursue my scientific career. Next on my dream list? A full Ironman. If I could run a half, why not a full? It took me almost three years to go from idea to project. I joined the Stanford triathlon team, led by two inspirational coaches, Bruce Smith and Gina Kehr, former Ironman champions. At this point, I had the CGM, which changed my way of managing my diabetes. In the Tri team, I was surrounded with the best athletes and coaches I ever dreamt of. My time had come! Last October, I sat with Gina, and said “I want to be an Ironman. I want to do it to raise awareness for type 1s”. She looked at me and said “Great! Let’s do it”.

This was the beginning of an epic adventure that started in October 2017 and ended in May 2018, in Santa Rosa, California. Eight long months of training every single day, several times a day! For any healthy athlete preparing an Ironman, the training plan is about educating your body to keep up for several hours. But for us Type 1s, it’s also about simulating each leg of the race while taking note of your blood glucose trends to find your best recipe for the race. Like an experiment, I tried and reproduced many protocols until I found the right one.
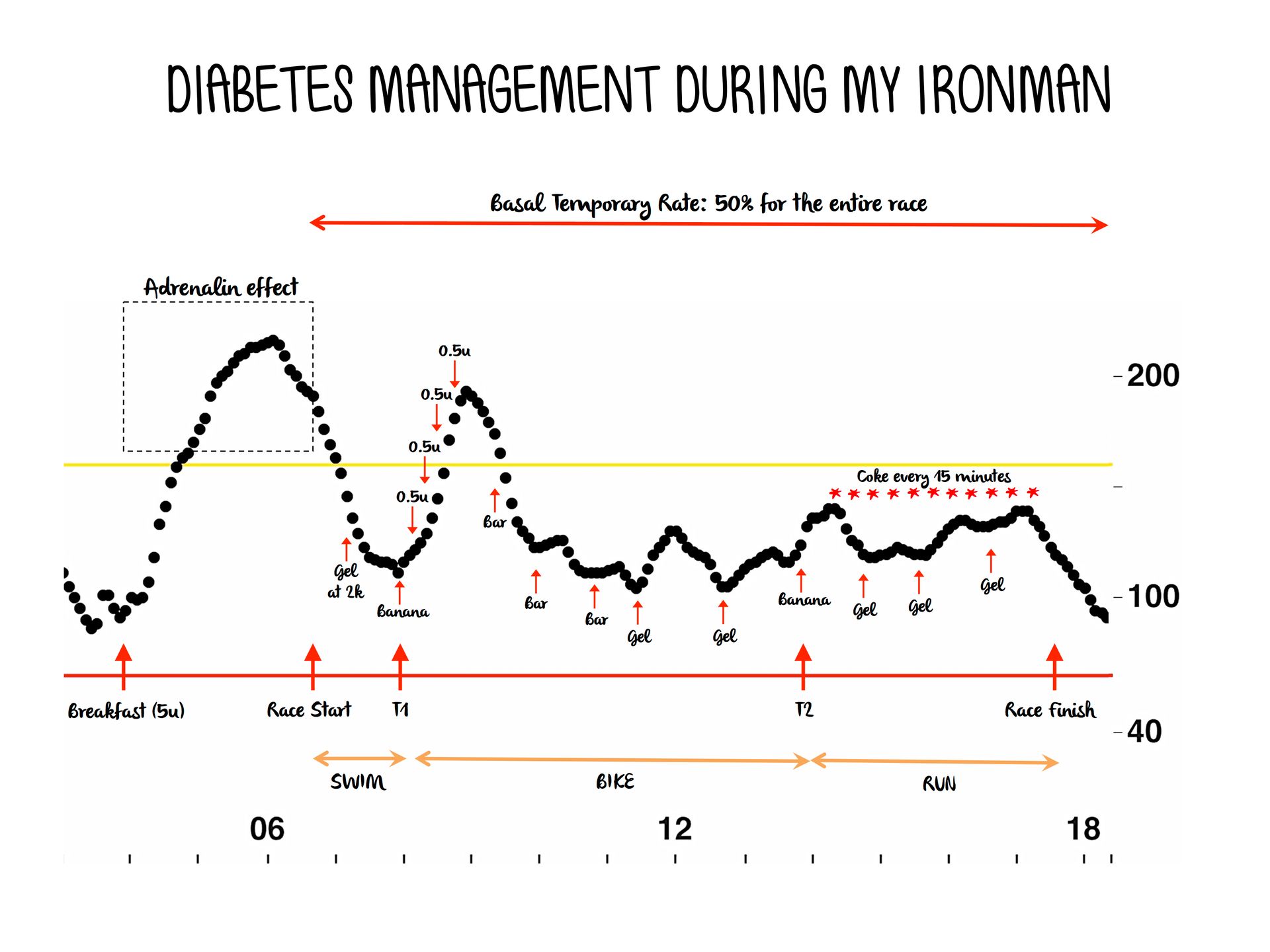
For my swim, I always noticed a drop around 1.2 miles (half of the distance of the race), therefore my trick was to take a gel after 35-40 minutes of swimming. For the bike, I figured out that riding with 50% of my basal was a good compromise to keep my BG in check. For the run, it was hard to define the best recipe since the best simulation was the race itself. As a rule of thumb, I decided to keep my 50% basal for the run, thinking I could disconnect my pump if ever my blood sugar crashed. I also simulated the effect of breakfasts, gels, bars, bananas, energy drinks on my BG while training. I kept simulating until the last week of training.
As the race approached, my family, my friends and colleagues were all asking me the same question: “Are you ready?” My answer was a solid “I am!” From the bottom of my heart, I knew I was: I had trained so hard and consistently; I had faced so many scenarios with my BG that nothing could happen to me. Yes, I was ready to fight!
During my entire training, I forced myself not to overthink how the race would go. I tried not to think about my goal time, nor to imagine myself crossing the finish line. I did not want to be too disappointed if something went wrong during the race. I was chasing the biggest athletic dream of my life, and I wanted type 1s to chase their owns. I started to share my training and my story on social media on @SweetT1dreams. My motto: let’s have dreams and make them sweet.
On Saturday May 12th 2018, my dream came true. After 10:51:42 of efforts, I became an Ironman. I nailed my blood sugars! (See the graph below). But more importantly, I tried so hard to advocate for type 1s with messages written on bandages during my run, that the guy with the microphone at the finish line said while I was crossing: “From France, Romain Ballet. You are an Ironman! Living with type 1 diabetes, you beat it young man! Yes you are, you are an Ironman”.

Being an Ironman is definitely one of the biggest achievements of my life. But ultimately, all of us share one common dream: finding a cure for type 1 diabetes! We depend on research for that and this is why I’ve dedicated my professional life as an immunologist to furthering this research. But research depends on public funds and therefore on you! At the beginning of my Ironman project, I set-up a fundraiser to support the work of the Children’s Diabetes Foundation. My goal was to reach $10,000. I have already collected $3,445 thanks to 52 amazing people. Amazing! But together, we can do more.
Dear friends, dear Type 1s: whatever the amount, even if it’s symbolic, go on this link and donate: https://www.youcaring.com/sweett1dreams-1135225. Thank you for your help! Thank you for reading my story, thank you for sharing.
Romain was diagnosed with type 1 in 2003 at the age of 16. His passion for teaching and science led him to become a Doctor in immunology with a focus on autoimmune diseases. He is currently a postdoctoral scholar at Stanford University. In addition to his contribution to research, Romain advocates for Type 1s by pushing his limits during long distance races such as Ironmans or marathons.









